TOG April 2019
Introduction
- Placenta plays an important role in development & growth of fetus
- Lesions in placenta can affect its function which leads to significant maternal/fetal morbidity
- Placental villous structural abnormalities correlate with time of onset of fetal growth restriction (FGR)
- Placental histology helps to know cause & predict recurrence risk of FGR
Guidance on indications for, and the process of, placental evaluation
Indications for placental evaluation

- Good practice to request placental histology if unexpected admission of baby to neonatal unit
- Extent of examination depends on clinical information provided, along with placental evaluation
Process for storing and sending placenta
- Store at 4°C in tightly sealed container
- Placenta shouldn’t be frozen
- Check criteria as for histology
- Use placental referral proforma
- Label container with patient’s details
- Submit to lab in fresh state
- Formalin fixation if likely delay in examination
Normal Placental development

Placental assessment in cases of adverse pregnancy outcomes
- 40% stillbirths are associated with FGR
- Knowledge of placental histology reduces the proportion of unexplained stillbirths
- Women should be counseled, while taking consent for postmortem, that placental examination can provide vital information to know the cause and help plan next pregnancies
- 1st systemic review (in 2014) confirmed that placental pathology led to stillbirth in more than 50% of cases
Placental changes in adverse pregnancy outcomes
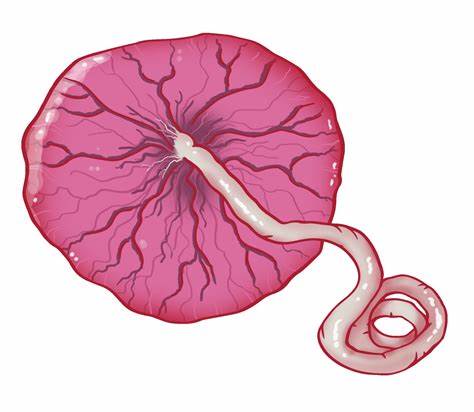
- Small placenta
- With a long and hypercoiled umbilical cord.
- Microscopy will confirm features such as
- advanced villous maturation,
- terminal villous hypoplasia,
- infarcts,
- decidual vasculopathy,
- massive perivillous fibrin deposition,
- fetal vessel thrombosis,
- chronic villitis of unknown aetiology and
- mesenchymal dysplasia
- Placental lesions are classified into three groups (by Redline in 2015)
- Vascular
- Immune
- Other comprising massive perivillous fibrin deposition (MPVFD), variations in placental shape & cord, placenta accreta and meconium-associated changes
Implications of key placental histological findings with reference to Amsterdam Placental Workshop Group Criteria
Amsterdam Placental Workshop Group criteria.
1. Maternal vascular malperfusion (MVM)
2. Massive perivillous fibrin deposition (MPVFD)
3. Fetal thrombotic vasculopathy (FTV)
4. Villitis of unknown aetiology (VUE)
5. Villous dysmaturity
6. Chorioamnionitis
Maternal vascular malperfusion (MVM)
- MVM belongs to group of placental vascular lesions
- It is a result of abnormal spiral artery blood flow associated with maternal conditions like preeclampsia
- Features are agglutinate villi, increased syncytial knots, distal villous hypoplasia (affecting >30% of distal villi) and infarcts
Distal villous hypoplasia aka terminal villus deficiency
- associated with post-placental hypoxia and FGR with absent or reversed end-diastolic flow
- microscopically, absent terminal villus side branches of mature intermediate villi and long, unbranched terminal capillary loops
- clinically, high Doppler resistance index
Massive perivillous fibrin deposition (MPVFD)
- Belongs to ‘other’ group of placental lesions
- Rare condition associated with perinatal morbidity/ mortality
- Can occur at ANY gestation
- Associated with recurrent miscarriage, FGR, stillbirth, preterm birth & neonatal neurological morbidity
- Excess fibrin & fibrinogen matrix surrounding atleast 30% of distal villi
- Also known as maternal floor infarction (MFI), BUT no signs of infarction histologically
- Aetipathogeneisis is not clear
- Macroscopically, placenta is yellowish, stiff & thick. Maternal surface looks corrupted with loss of cotyledons
- Microscopically, net-like pattern of fibrinogen that completely cover the villi. Then syncytiotrophoblast degeneration & fetal vessels obliterated. Fibrinoid heavily infiltrates the decidual floor, it leads to inter villous space obliteration
- Differential Diagnosis of MPVFD
- normal perivillous fibrinoid deposition
- chorionic villous ischaemia
- fetal thrombotic vasculopathy
- villitis of unknown aetiology
- MPVFD associated with significant adverse pregnancy outcomes
- FGR 24-100%
- Stillbirth 13-50%
- Recognized association with twin placentation & anti-phospholipid antibody syndrome
- Some studies report MPVFD
- Incidence: 0.28 per 1000 live births
- Recurrence: 12-78% (appropriate counseling of women for next pregnancy plan)
Fetal thrombotic vasculopathy (FTV)
- Belongs to ‘other’ placental vascular process
- Associated with cord abnormalities like hypercoiling, stricture, cord entanglement & long cord
- Prevalence of FTV 1- 6.4% (3.5% in placentas associated with adverse outcome)
- Aetiology: Unknown but could be associated with
1. hypercoagulable state caused by fetal polycythemia or maternal thrombophilia
2. endothelial cell injury caused by a true knot, abnormal cord insertion, long or hyper-coiled cord
3. blood flow stasis or turbulence within the placental vessels caused by cord entanglement or stricture
- FTV can occur as a result of placental or umbilical pathology
- Pathological changes include : avascular villi after occlusive thrombus, intimacy fibrin cushion, fibromuscular sclerosis and haemorrhagic endovasculopathy
- Changes in stillbirth and FTV are similar.
- In FTV changes are focal and clearly demarcated from adjacent structures
- In stillbirth changes are diffuse
- Macroscopically: subtle changes. Identifiable thrombus of grey-white colour with firm consistency
- Microscopically: thrombosis fetal vessels. Avascular villi confined to single villous structure
- Redline defined FTV in 2004 as, “presence of 15 or more avascular villi or villous stromal–vascular karryorhexis in two or more foci per slide in the absence of villitis of unknown etiology.”
- Avascular villi associated with FGR, oligohydramnios and fetal distress in labour
- FTV is associated with cord entanglement
- hypercoiling or other cord abnormalities
- maternal or fetal thrombophilia
- severe chorioamnionitis
- pre-eclamptic growth restriction.
Villitis of unknown aetiology (VUE)
- VUE belongs to group of placental ‘inflammatory’ immune processes
- Chronic inflammation with destructive changes and T cell infiltration into chorionic villi
- Inflammation may be patchy or diffuse
- VUE many be low or high grade
- VUE is common finding in 5-15% of near-term placentas
- Usually seen after 32 weeks gestation; any prior gestational association likely to be infectious
- Associated with FGR, recurrent pregnancy loss, neurodisability, twin discordance, idiopathic prematurity, hypertensive pregnancies, perinatal asphyxia, autoimmune and alloimmune diseases
- Higher risk of recurrence after index pregnancy but significance of recurrence is unknown.
Villous dysmaturity
- Belongs to group of ‘other’ placental vascular processes
- Well recognised association between villous dysmaturity and maternal diabetes (a study in 2008 showed that 80% of diabetic placentas had villous dysmaturity)
- Microscopically, terminal villi are enlarged, increased capillaries and macrophages, with fluid within villous structures
- Vasculosynytial membrane is increased in thickness which decreases maternal and fetal exchange of oxygen and other nutrients
Chorioamnionitis
- Belongs to groups of placental ‘inflammatory’ immune processes
- Defined as inflammatory process affecting chorion/amnion
- Higher in delivery at earlier gestation
- Inflammatory process is classified as
- Grade 1 (mild to moderate): individual or small clusters of maternal neutrophils, diffusely infiltrating the chorion laeve, chorionic plate, subchorionic fibrin or amnion
- Grade 2 (severe): ≥3 chorionic micro-abscesses (neutrophils confluence of at least 10×20 cells). Typically present in b/w chorion & deciduaa, +/- under chorionic plate
- Microbial invasion commonly occurs as a result of ascending infection rather than through blood
- PPROM & short cervix increase risk of amniotic infection
- Even with intact membranes bacteria can invade amniotic cavity
Placental histology: cost and medico-legal implications
- Financial and resource implications involved
- Cost implication must be balanced against valuable information provided by placental histology
- Referring hospitals must follow clear protocols
- Placental histology has vital role in medico-legal cases if adverse pregnancy outcome
Conclusion
- Placenta has key role in fetal/neonatal morbidity and mortality
- Obstetricians must understand the importance of placental examination if there is adverse pregnancy outcome
- Regular MDTs should be held to improve patient care in next pregnancy







