Q-Although Sri Lanka’s maternal mortality is the lowest in the South East Asian region it is still higher than in the developed countries.
Discuss the strategies which may be adopted to reduce this further.
- Introduction
- Maternal death -is the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the duration and site of the pregnancy, from any cause related to or aggravated by the pregnancy or its management but not from accidental or incidental causes. To facilitate the identification of maternal deaths in circumstances in which cause of death attribution is inadequate, a new category has been introduced: Pregnancy-related death is defined as the death of a woman while pregnant or within 42 days of termination of pregnancy, irrespective of the cause of death
- MMR- maternal mortality ration is the number of maternal deaths per 100000 live birth per year- in 2018 MMR 32 per 100000 live births.
- Srilanka has low maternal mortality rate when compared to other south Asian countries.
- But need to improved. According to SDG,
- At 2020 MMR 25
- 2025 – 15
- 2030 <10
- Strategies to reduce MMR
Pre-conceptional
- Ensure prevention, early Identification and management of direct and indirect causes of morbidities and mortalities to ensure optimal maternal, perinatal & neonatal outcomes.
E.g. School medical inspection- heart disease identification and referral
- Contraception if pregnancy is contraindicated.
Antenatal
- Early booking visit
- Now 83% <12 week booked at ANC
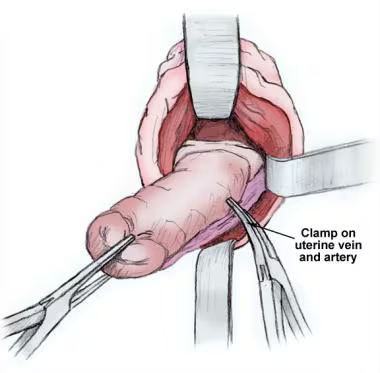
- Develop regionalized Highly specialized centers to manage women with severe obstetric complications eg: placenta accreta, eclampsia, heart disease complicating pregnancies etc
- Develop / strengthen MDT teams / clinics to manage obstetric complications and medical disorders complicating pregnancy with continuum of care
- Strengthen Referral, back referral systems and follow up of pregnant and post partum women eg: common pregnancy record – single record for a mother, communication system.
- Update / Develop/ implement national guidelines, protocols and standards for management of medical diseases complicating pregnancies and obstetric emergencies
- Established proper follow up programme
- Strengthen the linkages among Family Health Bureau, Epidemiology Unit, HEB and stakeholders for early identification and prompt action on epidemics such as influenza, dengue other communicable diseases
Intrapartum
- Increase hospital deliveries
- Currently 99.9% – it can increase almost 100%
- Further improvement of blood transfusion services – 24X7
- 24×7 laboratory facilities
Postpartum
- Increased awareness of contraception
- Prevalence of contraception usage 67%
- In 2018, 18% of maternal deaths are due to unmet need of family planning.
General
- Reduced teenage pregnancy rate
- Increased expenses to health system
- In SL 3.5% from GDP – in UK 17
- Evaluating quality of care for severe pregnancy complication
- WHO near-miss form
- Maintain f RED (register of eligibility women in danger) book