Discuss the strategies to reduce the perinatal mortality and morbidity associated with pre-term births in Sri Lanka. (100 marks)
This is a long answer. It also needs planning. However, most students will have a good knowledge of the area as it is a very common topic which would have been discussed many times during the clinical training.
In questions regarding prevention of morbidity and mortality, pre-conception, antenatal, intrapartum and postpartum methods of prophylaxis should be mentioned and it is the best and the easiest way to plan the answer. In this way a student without much knowledge can produce a reasonable answer. Do not forget to write a few words regarding PPROM and iotrogenic preterm delivery.
A good knowledge regarding preterm labour is needed to score distinction marks. Postgraduates should be very thorough with the most recent RCOG guidelines on preterm labour and PPROM to score pass marks. They should also be able to summarise their knowledge and write only the important points as the time is limited.
However the brighter side is that in this type of questions an undergraduate student with a very superficial knowledge can score pass marks as it has a wide answer.
Since it is a long answer be careful not to include unwanted details. Use short sentences. You should answer this question in the middle of the paper. If you cannot finish in the given time complete the answer at the end of the paper. Do not utilize extra time now as you should have time to attempt all questions.
A student with a trained mind and a little knowledge can score good marks in this type of questions. Therefore it is important to start training your mind to be quick and methodical. Imparting your knowledge to others is a good exercise in this regard.
ANSWER
Preterm delivery is birth before 37 weeks’ gestation. It is further delineated into very early preterm (before 32 weeks), early preterm (32 0/7 to 33 6/7 weeks), and late preterm (34 0/7 to 36 6/7 weeks) delivery.
Strategies to reduce perinatal mortality and morbidity and late complications from preterm labour should be carried out at the preconception clinic and the antenatal period together with early detection and proper management of preterm labour and expert neonatal care.
Identify risk factors for preterm labour at the pre-conception clinic or at the booking visit
- Previous preterm births./preterm pre-labour rupture of membranes
- Bacterial vaginosis.
- Twin pregnancy.
- Polyhydramnios.
- Uterine abnormalities.
- Cervical incompetence—congenital or acquired due to obstetric injuries, or surgeries such as cone biopsy, Manchester repair and cervical dilatation.
- Recurrent antepartum haemorrhage.
- Serious intercurrent illness.
- Smoking.
- Drug abuse.
- BMI less than 20.
- Teenage pregnancy.
- Low socioeconomic status
Prophylaxis during the pre-conception period
Women should be encouraged to attend the pre-conception clinic. Treat Intercurrent illnesses and give contraception till the disease is controlled. Stop smoking and drug abuse . Optimal BMI should be between 19-25. Encourage teenagers to use contraceptives. Treat UTI. Correct uterine abnormalities surgically before conception. Bacterial aginosis may have to be excluded or teated in those with recurrent preterm births.
Avoid cervical surgeries or avoid damaging the area of the internal os in women of the childbearing age. Dvise cerical circlage during pregnancy for such women.
Prophylaxis during the antenatal period
Prophylactic measures for women with a singleton pregnancy at risk of preterm birth.
- Perform transvaginal USS from 16-24 weeks to assess cervical shortening.
- Vaginal progesterone or cervical circlage is recommended for women with:
- A history of spontaneous preterm birth or mid-trimester loss between 16+ and 34+0 weeks of pregnancy
and
- A cervical length of less than 25 mm in the transvaginal ultrasound between 16+0 and 24+0 weeks of pregnancy
- Vaginal progesterone 200 mg are inserted daily till 34 weeks for women with a cervical length of less than 25 mm, without a history of spontaneous preterm birth or mid-trimester loss.
- Prophylactic cervical cerclage is indicated for women whose cervical length is less than 25 mm and who have either:
- had preterm pre–labour rupture of membranes (P-PROM) in a previous pregnancy or
- a history of cervical trauma
‘Rescue’ cervical cerclage
This is considered for women between 16+0 and 27+6 weeks with a dilated cervix and exposed, unruptured fetal membranes.
‘Rescue cervical cerclage is contraindicated in the presence of :
- Signs of infection or
- Active vaginal bleeding or
- Uterine contractions.
Cervical circlage should be performed by an experienced surgeon and should be inserted close to the internal os.
The above methods are not recommended for multiple pregnancies. Preterm labour cannot be predicted or prevented in twin pregnancies.
Prevent polyhydramnios by early detection of fetal abnormalities and isoimmunisation and treatment of diabetes.
Early diagnosis and management:
Early diagnosis is helpful to prevent progress, to administer tocolytics and corticosteroids and to arrange for specialized neonatal care.
Diagnosis is suspected if :
- There is a history of colicky lower abdominal pain, backache and show. In most cases the symptoms are vague.
- Examination reveals palpable painful uterine contractions. Speculum examination may reveal cervical dilatation. Avoid VE as it can release prostaglandins
- There are regular uterine contractions on the cardiotocograph.
Perform a streile speculum examination to exclude PPROM.
Clinical assessment alone may be used to diagnose preterm labour before 30 weeks.
Preterm labour is confirmed after 30 weeks if:
- The cervical length is less than 15 mm or
- Fetal fibronectin level is more than 50 ng/ml (this test is indicated if measurement of cervical length is not performed)
Inform the neonatal team. It may be necessary to transfer to a hospital with good neonatal care.
Treatment with corticosteroids:
- If the POA is between 26+0 and 33+6 weeks give 2 doses IM betamethasone 12 mg 12 hours apart, or 4 doses of 6 mg of dexamethasone 12 hours apart, to enhance lung maturation. Consider between 24+0 and 25+6 weeks and between 34+0 and 33+6 weeks
Corticosteroids are most useful if delivery occurs between 48 hours-one week. Repeat courses are not advised.
Use of tocolysis:
Nifedipine is the drug of choice.20mg is given initially. The maintenance dose is 10–20 mg every 4-8 hours up to 48 hours and the dose is adjusted according to uterine activity. The total daily dose should be below 60mg.
Intravenous magnesium sulphate:
Give 4 gm over 15 minutes, followed by an intravenous infusion of 1 g per hour until the birth or for 24 hours (whichever is sooner) for neuroprotection of the baby, between 24+0 and 29+6 weeks ( consider also from 30- 33+6 weeks).
Monitor for clinical signs of magnesium toxicity at least every 4 hours by recording pulse, blood pressure, respiratory rate and patellar reflexes.
Preterm prelabour rupture of membranes:
This is diagnosed by demonstrating pooling of liquor by sterile speculum examination.
If liquor is not seen perform an insulin‐like growth factor‐binding protein 1 or placental alpha microglobulin‐1 test of vaginal fluid
Observe for signs of chorioamnionitis or fetal distress
- Maintain a temperature chart 4–8 hourly to exclude pyrexia.
- Auscultate the fetal heart rate 4–8 hourly for tachycardia.
- Inspect pads for offensive, purulent vaginal discharge or meconium.
- Perform a high vaginal swab at the initial speculum examination to exclude infection.
- Perform full blood count and C-reactive protein.
- Cardiotocography is useful as fetal tachycardia can be due to chorioamnionitis.
Give oral erythromycin 250 mg 4 times a day for a maximum of 10 days or until delivery (whichever is quicker).
If there is no fetal distress or infection pregnancy can be continued till 37 weeks.
Fetal monitoring :
- Cardiotocography is performed.
- A normal cardiotocograph trace is reassuring and indicates that the baby is coping well with labour, but an abnormal trace does not necessarily indicate that fetal hypoxia or acidosis is present.
- Do not use a scalp electrode or perform fetal scalp blood sampling if the POA is less than 34 weeks.
Delivery and neonatal care
- Vaginal delivery is allowed.
- There is no added advantage of performing a caesarean section.
- Perform continuous fetal heart rate monitoring.
- Perform lift out forceps delivery to protect the head from sudden decompression.
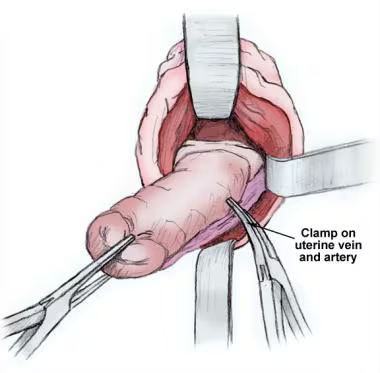
- LSCS is done for preterm labour between 26+0 and 36+6 weeks with breech presentation.
Iotrogenic preterm delivery:
Aoid delivery before 37 weeks except to save the mother or the baby. Give corticosteroids in all such cases. Confirm dates in every woman between 9 -22 weeks to prevent inadvertent preterm induction or LSCS.
Improve neonatal care
Expert neonatal care is essential to reduce the mortality and morbidity. The pediatric team should be present at delivery and advanced neonatal support is necessary. Transfer to a specialized unit once preterm labour is suspected,
Preterm delivery can recur in the next pregnancy. Therefore careful TVS for cervical shorteninig should be done from 16 weeks.
Reference:
SBA Questions in Obstetrics by Eranthi Samarakoon, chapter 15
Preterm labour and birth NICE guideline [NG25] Published date: 20 November 2015 Last updated: 02 August 2019
Most of the pregnancy related complications can be minimized or prevented by proper pre pregnancy counseling. Discuss this statement.
(University of Rajarata ) (Suitable for postgraduates also)
Pre-pregnancy counseling involves counseling a woman before pregnancy commences, about her personal heath, the course and outcome of pregnancy and possible complications. This can be done at a routine medical checkup, clinic visit for contraception soon after marriage or a pre-pregnancy visit. All women should be motivated to undergo a pre-pregnancy medical checkup at the local MOH clinic
The objective of this is to ensure that a woman enters pregnancy with optimal health which is best for her and her baby. During this examination, any risk factors that could affect both mother and baby are identified and treated. This is especially important for women with, chronic illnesses, known risk factors or a history of pregnancy failures.
Most of the baby’s major organs and systems complete their development by 10 weeks. Mother’s health and nutrition can affect this initial crucial development. Therefore, it is essential to correct and treat adverse health issues before embarking on pregnancy.
During this visit a detailed history of the couple which includes their medical, personal, family and obstetrical history is taken. This helps to identify any risk factors they have. A thorough physical examination and relevant investigations are done and treatment is provided for any illnesses which are detected.
Benefits of pre-conception visit include:
- Planning of optimal time for pregnancy and prevention of unplanned, unwanted pregnancies
- Immunization
- Promotion of healthy behaviors .
- Ensuring optimal weight and nutrition
- Prevention of birth defects
- Prevention of low birth weight (LBW) and prematurity
- Optimizing medical disorders and adjusting drug therapy
- Optimizing mental health
- Advise regarding antenatal clinic visits
- Prevention of poor pregnancy outcome recurrences
- Preparation for breast feeding and parenting
A suitable method of family planning should be given for spacing of pregnancies and till the couple is ready for a pregnancy. Mothers may attempt termination of unwanted pregnancies with resultant sepsis, chronic ill health and infertility or may neglect herself during such a pregnancy.
Inform couples that it is better to complete the family before 35 years because of the risk of trisomies.
Prevent grandmultiparity with suitable contraception.
Women who have not been vaccinated against rubella and hepatitis B should be vaccinated and given contraceptives for three months to prevent serious fetal consequences of these diseases.
Test the couple for HIV, hepatitis B and syphilis as vertical transmission can occur if the woman is infected. Test the woman for chlamydia and gonorrhea as these can cause PID with resultant ectopic pregnancy. Perform cervical smears in untested women.
Women should avoid:
- Smoking , alcohol, addicting and unprescribed drugs before pregnancy as these habits can result in birth defects, LBW, pre-eclampsia and placental abruption.
- Exposure to agricultural and other toxins.
- Having unprotected sex with multiple partners because of the risk of acquiring STDs
Optimal weight and hemoglobin level is necessary for a normal pregnancy. A woman should control her diet and engage in exercise to start her pregnancy at a normal BMI of between 18.5 and 24.9. Obesity can cause many problems such as GDM, pre-eclapmsia and preterm labour.
Anaemia can cause maternal ill health SGA babies and aggravate the effects of even the normal blood loss at delivery. The Hb should be at least 12 g /dl at the start of pregnancy. Advise regarding a balanced diet.
Educate women with medical complications about the effects of the disease on pregnancy and also effects of pregnancy on the disease. Pre-existing chronic diseases (hypertension, heart disease, connective tissue disease diabetes, epilepsy) should be stabilised in an optimal state.
- Perform a MDT assessment of the medical condition.
- HbA1c should be 6.5, diabetic nephropathy and retinopathy should be treated
- BP should be less than 130/85
- Cardiac disease should be treated and in NYHA grades 1 or 2
- Epileptics and women with connective tissue disease .should be on least toxic drugs.
In some cases these diseases may be diagnosed for the first time at the pre-conception clinic
Drugs used before pregnancy are verified and changed if required to avoid any adverse effects on the fetus. Glibenclamide, angiotensin converting enzyme inhibitors, angiotensin receptor blockers, sodium valproate, statins, cyclophosphamide, methotrexate and diuretics are some of the drugs which should be replaced by less toxic drugs
In severe disease conditions postpone or discourage conception. Recurrent fits, recurrent flares or multi organ involvement of SLE, severe diabetes with HbA1c more than 10, are some of these. Pregnancy is contraindicated in cyanotic heart disease, Marfan’s syndrome and pulmonary hypertension
If a couple have a personal history of a inheritable disease or has produced a child with such a disease or if the woman is over 35 years, chances of producing an abnormal child can be discussed and arrangement for early detection can be done. Perform prenatal genetic testing for parents who may be carrying a translocation or an autosomal recessive or a dominant disorder. Advise early pregnancy tests such as PAPPA –A levels, hCG levels, nuchal translucency, cell free DNA tests or second trimester biochemical tests if the woman is at risk of aneuploidies.
If a patient has a history of a previous still birth or recurrent miscarriages try to find out the cause and treat it if possible. Perform anticardiolipin antibodies to exclude antiphospholipid syndrome.
Eliminate major or minor risk factors for LBW.
Advise women with the risk factors for pre-eclampsia to commence aspirin at 12 weeks or pre- pregnancy if the risk is very high.
Advise those with a past history of preterm labour to perform TVS from 16-24 weeks.
Correct thyroid dysfunction before pregnancy and give iodine and folic Acid supplementation as deficiencies in both substances can affect the brain development of the baby. Give folic acid 5 mg should be given for diabetics, epileptics and those with a previous baby having a NTD.
Couples should also be advised regarding:
- Good mental health of the mother and avoidance of domestic violence
- The need for regular antenatal visits
- Breast feeding. Breasts should be examined to exclude masses and retracted nipples.
QUESTION 13
Discuss the measures which could be adopted to reduce the incidence of teenage pregnancies in Sri Lanka.
(University of Ruhuna)
REVIEW
This is a general question which can be answered very well without much knowledge of the subject. Only general knowledge and a little imagination are required to answer this question very well. The definition is obvious as a teenager is a child under the age of 20 years. The incidence is not essential to score good marks. The reasons for the occurrence of teenage pregnancies are within the knowledge of even non- medical people.
ANSWER
The negative obstetric and fetal outcomes as well as social consequences associated with teenage pregnancies are well documented globally and regionally. Preventing teenage pregnancy is important in achieving the millennium development goals of maternal and child survival.
A pregnancy occurring in a young woman who has not reached her 20th birthday is considered as a teenage pregnancy. This definition is applicable irrespective of the legal status of the marriage of the woman or legal age to consider an individual as an adult.
Teenage pregnancy rate in Sri Lanka is much lower than the rates in other South Asian countries. Reproductive health information database of Family Health Bureau of the Ministry of Health, Sri Lanka, indicate that it is 6.5% of the total pregnancies.
The reasons for teenage pregnancies include:
- Lack of sexual education
- Lack of knowledge regarding contraceptives
- Premarital sex
- Low education level
- Poor parental support
- Poor support from teachers
- Low socio-economic status
- Accepted teenage marriages in certain ethnic groups
- Restrictions regarding dispensing contraceptives to adolescents
- Disrupted family status
- Addiction to drugs and alcohol
- Use of internet and face book
- Sexual abuse
- Having had teenage parents
- Being in the care of social services
- Poor transition from school to work at 16 years of age
- Mental health problems
To prevent teenage pregnancies all the above should be eliminated. This will need the combined efforts of the government, teachers, parents, community midwife, social service organisations, family health bureau, police, clergy and the entire community.
Our teenage children have not been exposed to sex education and are hence unaware of the dangers of unprotected sexual intercourse and the availability of contraceptives.
Sex education plays a major role in primary prevention. This topic should be included in the curriculum at the middle school level. Children should know about the menstrual cycle, ovulation and the risk of pregnancy and risk of contacting STDs if they engage in unprotected premarital sexual intercourse with casual short term acquaintances.
Knowledge about contraception and availability are very important preventive measures. There should be legislation to dispense contraceptives freely irrespective of age and without parental permission.
The midwife has a role to play as most of the teenage children are not aware of sex education and contraception. She should hold regular educational meetings with the parents and children during week ends. Give contraceptive advice to young couples before marriage. They should be aware of COCP and condoms which should be freely available. Adise young girls regarding emergency contraception. Those who start employment in factories and such places at an early age should be educated regarding the dangers of unprotected pre-marital sex and availability of contraception. There should be regular lectures from the MOH and the midwife of the area.
Family support is essential for adolescents. Teenage children from broken families and where the mother has gone abroad for work can fall prey to unscrupulous men. The government should bring legislation to prevent women with under-aged children from going abroad for employment.
Mothers who are working may not be able to track the movements of their daughters, but father, mother and extended family members should always be aware of the time their daughters leave and come home.
Unlike in other Asian countries teenage marriages are not a common or an accepted norm. Adolescent girls should be encouraged to persue their studies and marriage should not be a priority. Teenagers had to leave school if they cannot get enough passes in the OL examination to proceed to the AL class but now the government has introduced a system where such children can proceed to the AL class. Teachers have a major role in preventing school drop outs as most of the teenage pregnancies occur among such children.
Less educated people among certain ethnic groups encourage early teenage marriages. The age of marriage should be raised to 20 years to prevent early marriages.
Large tuition classes are places where young children meet and make casual relationships which may end up in sex and pregnancy. Both parents and teachers should be more vigilant about the attendance of the children and parents should make sure that children actually attend the class and reach home at the correct time. Most of the teachers are mercenary and are indifferent about the welfare of the children and are not happy to maintain a dialogue with the parents.
There should be strict government rules to curb drug addiction among school children.
Low education level and poor socio economic status of the parents also favour teenage pregnancies. Such families may live in the same yard or in line rooms or similar houses which favour relationships. Men as well as young boys in such neighbourhoods are addicted to alcohol and drugs. Police should be vigilant to prevent such pratices.Also young children who have dropped out of school and are unemployed will form relationships as they are at home throughout the day often without parental supervision. Sexual abuse also can occur in such situations. Some form of free education should be available for teenaged children. Parents should form groups to at least take turns to be more vigilant in such situations.
Clergy also have a role to play. They can encourage religious and social activities to keep the children occupied. They should also instill good practices in keeping with our culture. Mentally retarded and depressed children need more protection as they can “willingly” or unwillingly fall prey to sexual abuse.
There should be strict rules to prosecute and punish offenders of sexual abuse. Police should frequent cinema halls, lodges and parks and apprehend young teenagers who come to such places after leaving home to go to school or classes.
Children should not be given phones with internet facilities. Use of internet at home should be allowed only under the supervision of the parents.
The social stigma associated with pre -marital sex and out of wedlock pregnancies result in the child not revealing the incidence. Also the rules prevent termination of such pregnancies unlike in other countries. These children may seek illegal abortions with resultant serious health hazards.
Social service organisations should form societies among young children and advise them regarding sex education.
The entire society has a role to play to protect our young children and to prevent unwanted teenage pregnancies.
Reference:
Review Management of teenage pregnancy Authors Richard P Horgan / Louise C Kenny