- Preparations
- UKMEC3/4
- Mode of action
- Failure rate
- Return of fertility
- Discontinuation
- Side effects
- Health concerns
- Drug interactions
- Non-contraceptive benefits
Oral contraceptive pills
OCP
- Combined OCP
- Monophasic
- Biphasic
- Triphasic
- Low dose estrogen
- High dose estrogen
- Cyclical usage
- Extended usage
- 2nd generation progestogen
- 3rd generation progestogen
- Progestogen only pills POP
- Emergency contraceptive pills ECP
Injectable contraception
- DMPA
- Proluton
Contraceptive devices
- Copper IUCD
- Hormonal IUCD
- Mirena- levonorgestrel
Barrier methods
- Condoms
- Diaphragm
Sterilization
- Female sterilization
- Male sterilization
- Vasectomy
Natural methods
Contraceptive methods
Oral contraceptive pills OCP
- Combined OCP
Failure rate – 0.2-3 per 100 (typical use 9%, perfect use 0.3%)
Mode of action
- Suppress ovulation
- Reduces sperm permeability by thickening cervical mucus
- Alters endometrium and reduces the likelihood of implantation
Side effects
- Nausea and vomiting
- Dizziness
- Breakthrough bleeding / irregular bleeding
- Breast tenderness
- Headache
- Weight gain
- Monophasic
- Same dose of drugs throughout period Biphasic
- Two amounts/doses of estrogen and progesterone
- Same dose of drugs throughout period Biphasic
- First 10 days and next 11 days
- Triphasic
- Three amounts/doses of estrogen and progesterone
- First 7 days middle 7 days and last 7 days differ
- Low dose estrogen
- 30ɥg of ethinylestradiol- now common
- High dose estrogen
- 50 ɥg of Mestranol
- Taken for 21 days with pill free interval (PFI)/ non hormonal tablets
- Taken continuously without pill free interval
- Ethinyl estradiol 20-35 ɥg + levonorgestrel 150 ɥg derrivatives
- Ethinyl estradiol 20-30ɥg + Desogestrel/ gestodene 0.075 mg/ norgestimate
- Ethinyl estradiol 30ɥg+ Drospirenone 3mg
- Diane 35
- Ethinyl estradiol 35ɥg+ Cyproterone acetate 2 mg
- High dose estrogen
- Monitoring in COCP (follow up)
- Review after starting in 3 months
- Measure BP every visit.
- Measure BMI every visit.
- Progestogen only pills POP
- Useful for premenopausal women and breast feeding women
- Failure 0.4-4 per 100
- Emergency contraceptive pills
- Norethisterone 0.35 mg

| COCP | Progesterone only pill (POP) |
| Mechanism of action Inhibit ovulation, sperm permeability and implantation Alters levels of FSH and LH by pituitary | Inhibit sperm permeability and implantation. Ovulation inhibited by 50% only-reason for irregular spotting, does not alter FSH and LH level easy to detect menopause. |
| Taken for 21 days and 7 day PFI- withdrawal bleeding (action last for 7 days if taken continuously for prior 7 days) | Taken every day without PFI |
| Less strictness for timing of tablet- even in 7 day withdrawal PFI action is sustained. | Strictly adhere to timing of pill- action decays throughout 24 hours, after 27 hours (3 hour delay) failure rate high so need additional method for up to 2 days. |
| Benefits Prevention from cancers- endometrial cancer risk reduction 50%, ovarian cancer risk reduction 12 to 8 per 1000 (protection increase with duration of use and persists for 30 years), reduction of colorectal cancer. Reduces acne vulgaris. Reduces Rheumatoid arthritis 30%. Reduces PID. Reduces rate of ectopic pregnancy. Risks Arterial disease- increase risk of MI Slightly increases BP (but within normotensive range) Increases the ischemic stroke in Migraine with aura. Small increases VTE. (risk increase with 3rd generation progesterone than 2nd generation) Small increase in breast cancer- risk reduce to 0 after stopping for 10 years. Very small increase in cervical cancer. | Benefits No estrogen- no risk of MI, Stroke, migraine and cancer risks. Less progesterone than COCP- no side effects of progesterone. Easily reversible than COCP. Risks Strict adherence to pill timing. Unpredictable bleeding pattern. Functional ovarian cysts. Risk of ectopic pregnancy high compared to COCP- ovulation occurs. |
| Contraindications Morbidly obesity (BMI>40) Uncontrolled HTN (>160/ 95) Migraine with aura at any age. >35 years with smoking (>15 cig/day) Thrombophilias MI/Stroke/DVT- on anticoagulation or past history. Current breast cancer GTN After major surgery+ immobilization Avoid up to 6 months breastfeeding | Contraindications Multiple circulatory risk factors. |
Non-contraceptive benefits of COC
| uterine | ovarian | extra-genital | |
| possible protective | |||
| Dysmenorrhea Blood loss. Regularize PID PMS endometrial CA 50% | incidence of functional ovarian cysts, benign ovarian tumours, PCOS ovarian CA 50% | 1.Acne 2.Benign breast disease 3.Hirsutism | rheumatoid arthritis, thyroid disease and duodenal ulceration. Colorectal CA |
Potential benefits of combined hormonal contraception (in order of strength of evidence)-TOG 2012
- 50% reduction in risk of ovarian and endometrial cancer.
COCs reduce three major histologic types of endometrial cancer:
- adenocarcinoma,
- adenosquamous carcinoma and
- adenoacanthoma
- Improvement in acne.
- Reduction in heavy menstrual bleeding.
- Regulation of menstrual cycles.
- Alleviation of dysmenorrhea.
- Treatment of hirsutism and polycystic ovary syndrome.
- Treatment of premenstrual syndrome.
- Reduction in risk of colorectal cancer.
Starting COCP
- 1-5 days of menstrual cycle- no need for extra protection but after day 5 need for 7 days.
- Within 21 days after child birth- no need for extra protection
- Within 1-7 days after miscarriage or termination <24 weeks.
- If amenorrhoea, at any time if pregnancy excluded- extra protection for 7days.
- Post partum+ not breast feeding+ >21 days+ normal menstruation= as in normal women.
Post partum+ breast feeding+ <6 months= not recommended COCP,
>6 months, normal menstruation same as in normal non pregnant woman.
Progestogen only Injectable contraception-EBM
| Preparation | IM DMPA | S/C DMPA | NET-EN |
| Depot medroxyprogesterone acetate | (Sayana Press) | Norethisterone enanthate | |
| 150 mg IM | 104 mg | 200 mg | |
| 12 wk | 13 wk | 8wk | |
| 3 monthly, needs to return in 13 weeks Can be given upto 7 days delay -without an additional method WHO-effective up to 17 weeks | |||
| Preferred site- Gluteal Deltoid- also possible 2ml syringe 21-23 FG IM needle | Upper ant thigh or ant abdomen SC-special formulation of DMPA | ||
| Rates of bone loss, amenorrhea, weight gain, return of fertility similar | |||
| UKMEC 3 | CVS Dx -multiple risk factors for arterial CV Dx HTN-Vascular Dx Current & H/O IHD & Stroke Unexplained vaginal bleeding Breast CA- past & no evidence of Dx for 5yrs Diabetes- nephro/retino/neuro + other vascular Dx Cirrhosis- severe (decompensated) Liver tumors-hepatocellular adenoma+ malignant hepatoma SLE: + or unknown AB | ||
| UKMEC 4 | Breast cancer- current | ||
| Mode of action | Inhibition of ovulation Thickening of cervical mucus Unfavourable endometrium | ||
| Failure rate | <4/1000 over 2 yr | typical use 6% | |
| Return of fertility | Upto 1 yr. Long term reduction in fertility- no evidence | ||
| Discontinuation | 50% in 1 y. Bleeding issues + weight gain | ||
| Side effects | Amenorrhea 1/3 at 3/12 70% by 1 yr Weight gain- average 2-6kg. More BMI >35 than <25 Hair loss Irregular bleeding Delayed return fertility 6-18 months delay in starting ovulation (average 4 months) | ||
| Health concerns | CVD BMD | ||
| Drug interactions | Enzyme inducing drugs- DO NOT↓ Injection intervals- same | ||
| Non contraceptive benefits | Improves dysmenorrhea Endometriosis symptoms ↓ menstrual blood loss Improvement in anemia ↓ frequency sickle crisis | ||
DMPA
- Progesterone only contraceptive
- Contain medroxyprogesterone acetate 150 mg Given intramuscularly 12 weekly If delayed more than 14 weeks, additional protection must be given for 7days.
- Mechanism of action
Prevent ovulation, prevent sperm penetration by altering cervical mucous and thinning of endometrium
| Advantages | Disadvantages |
| Prevents endometrial cancer, PID, fibroids and endometriosis. | Irregular bleeding up to 12 months then amenorrhea |
| Need less compliance | Prolong use might reduce bone mineral density- cautious in young and old women. |
| Stabilizing effects on epilepsy, sickle cell disease and women taking liver enzyme inducing drugs. | Weight gain in obese women Bloating, mood change, headaches progesteronic side effects |
| Return to the fertility may be delayed |
DMPA is a long-acting, synthetic, progestin-only injectable contraceptive that suppresses ovarian estrogen, leading to a reduction in the synthesis and secretion of ovarian estradiol
hence long-term users commonly have plasma estradiol levels that are at or below normal levels in the early follicular phase. As estradiol is important in bone maintenance, the concern is that its suppression may lead to osteopenia and ultimately cause an increase in risk of fractures in older women. Loss of BMD in the case of DMPA has been associated with estrogen deficiency.
- Proluton
Subcutaneous implants
- Implanon
- Contains etonorgestrel 68 mg, 20-30 micrograms per day release.Very less failure rateLicensed for 3 yearsPrimary action
-
- ovulation inhibition,
- then inhibition of sperm permeability and thinning of endometrium. (ovulation suppression achieved through inhibition of LH not the follicular function).
- Subdermal implants
- 20% experience amenorrhoea,
- ¼ remove due to irregular bleeding within 1 year.
- side effects of progesterone
- mood changes, weight change, loss of libido, bloating, breast tenderness and headaches.
- No risk of VTE or reduced bone mineral density.
- side effects of progesterone
| Preparation | Nexplanon/ implanon | Norplant | Jadelle |
| Nex bioequivalent to implanon | |||
| 1 rod 68 mg ENG in a membrane of ethylene vinyl acetate | 6 rod LNG | 2 rod LNG 2*75mg LNG | |
| Nex-Radio-opaque (BaSO4) daily dose – 60-70mcg /day is released 2nd yr- 35-45mcg/day 3rd yr 30-40mcg/day | 100mcg/day- by 1st month 40mcg/day by 1st yr 30mcg/day by thereafter | ||
| 3 yr | 5 Yr | 5 Yr | |
| UKMEC 3 | Current & H/O IHD & Stroke Unexplained vaginal bleeding Breast CA- past & no evidence of Dx for 5yrs Cirrhosis- severe (decompensated) Liver tumors-hepatocellular adenoma+ malignant hepatoma SLE: + or unknown AB | ||
| UKMEC 4 | Breast cancer- current | ||
| Mode of action | Inhibition of ovulationThickening of cervical mucusUnfavourable endometrium | ||
| Failure rate | <1/1000 over 3 yr (0.05%) | ||
| Return of fertility | |||
| Discontinuation | 43% in 3 y. Bleeding issues (1/3) other reasons (<10%) | ||
| Side effects | Amenorrhea 20% Weight gain- 3-12% Mood changes Loss of libido Acne-↑↓↔ Headache-no relationship | ||
| Health concerns | VTE-no ↑ BMD-No evidence SABE prophylaxis- No need | ||
| Drug interactions | Enzyme inducing drugs likely to ↓ effectiveness Anticonvulsants, anti-retrovirals, rifampicin, rifabutin Therefore CONSISTENT USE OF CONDOMS | ||
| Complications of removal | <1% Deeply sited, non-palpable, broken, migrated | ||
Contraceptive devices
Copper IUCD
- Act by preventing implantation by causing inflammatory reaction in endometrium and toxic to the sperms and ova (prevent fertilization)
| Advantages | Disadvantages |
| Rapidly reversible | Risk of PID if woman have STI At the time of insertion only. High risk include, <25 with new sexual partner or 2 or more partners within last 1 year. Prophylactic AB is indicated in this group only. |
| Long duration of action 5-10 yrs | Risk of HMB and dysmenorrhea 50 % remove at 5 years |
| Used as emergency contraception for 5 days | Uterine perforation at the time of insertion (1-2/1000) |
| Prevents endometrial cancer | Ectopic rates high but lower than non contraceptive users. |
Levonorgestrel IUCD
- Mirena-52mg levonorgestrel- 20 micro per day release
- Mechanism of action-
- inhibit fertilization and implantation, does not prevent ovulation in majority of cases.
- Can take up to 7 days of menstruation or after pregnancy exclusion
- Action is not immediate
Licensed for use for 5 years
| Advantages | Disadvantages |
| Reduces HMB/blood loss, endometriosis associated dysmenorrhea and fibroid associated blood loss | Perforation, expulsion and infection. |
| Very effective– 20% will experience amenorrhoea by 1yr | Irregular bleeding for 6 months but after one year usually amenorrhoea. |
| Very little systemic side effects. |
Barrier methods
- Condoms
- Diaphragm
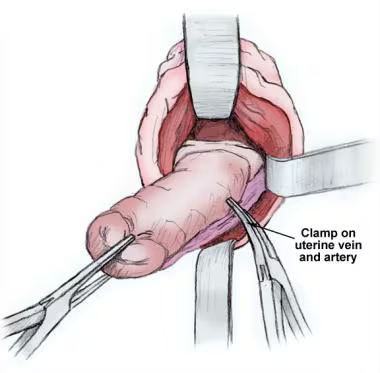
Sterilization
- Female sterilization
- Male sterilization
- Vasectomy
Natural methods
- Coitus interruptus
- Fertile period avoidance
Spermicides
Situations of use
- Newly married delaying fertility
- Post partum contraception
- Family completed
- Contraception in medical disorders
- Missing pills
- COCP
- Missed one tablet- no take it immediately no need for other contraception
- 2 or more (20 micrograms)/ 3 or more (30 micrograms)- take pill ASAP and use other contraceptive method for 7 days.
- If pills missed in First 7 days of card- use emergency contraception
- if sex in last 7days (PFI longer)
- If pills missed in middle 7days- ideally no need for emergency contraception.
- If pills missed in last 7 days- finish the pills in current pack and start new pack straight away (Avoid PFI then no need for emergency contraception)
- COCP
- Emergency contraception
- Endometriosis
- AUB