It has been revealed during the 2016 maternal death review that there have been maternal deaths due to failure to provide PPFP
12.1 What do women need to know about PPFP. (25 marks)

What can be done to improve the opportunities for providing PPFP?
Postpartum family planning is defined as the prevention of unintended pregnancies and closely spaced pregnancies through the first 12 months following childbirth. [WHO-2013]
•Worldwide, more than 9 out of 10 women want to avoid pregnancy for 2 years after having had a baby, but 1 in 7 of them is not using contraception.
•PPFP can save mothers’ lives – family planning can prevent more than one-third of maternal deaths.
PPFP can also save babies’ lives – family planning can prevent 1 in 10 deaths among babies if couples space their pregnancies more than 2 years apart.
•Closely spaced pregnancies within the first year postpartum increase the risks of
- Preterm birth,
- Low birthweight and
- Small-for-gestational-age babies.
•The risk of child mortality is highest for very short birth-to-pregnancy intervals (i.e. less than 12 months).
•The timing of the return of fertility after childbirth is variable and unpredictable. Women can get pregnant before the return of menstruation.
The purpose of a comprehensive PPFP service is to help women to choose the contraceptive method they want to use, to start that method, and to continue to use it for 2 years or longer, depending on their reproductive plans.
2018- UNFP of total maternal deaths

PPFP should be discussed at every opportunity. If you can, you should start to discuss PPFP while the
woman is still pregnant so that she is able to start her chosen method as soon as possible after delivery.
| Avoiding missed opportunities for PPFP | ||
| In the antenatal clinic | Women should be given verbal and written information about all PPFP options. Women should be told about the particular benefits of PPFP, particularly of intrauterine devices (IUDs) and implants. For women who are considering limiting their family size, it may be appropriate to discuss vasectomy or female sterilisation with the woman and her partner at this time. For women who are considering limiting their family size and undergoing a planned caesarean section, the possibility of concurrent tubal ligation should be discussed. Women should be given the opportunity to ask questions about contraception every time they are seen in the antenatal clinic. The method that the woman has chosen should be documented in the appropriate case record so that it can be provided as soon as possible after childbirth. If hormonal pills or barrier methods are chosen, these could be provided during late pregnancy so that women have a supply at home to start at the appropriate time after childbirth. | Healthcare providers who provide antenatal care should be given the time and opportunities to be trained to give contraceptive advice. Discussion of contraception can become part of any antenatal visit but becomes more important for method selection as the woman approaches term. To ensure that it is being discussed, ‘Contraceptive advice’ can be added to maternity checklists. Women can be provided with information (in a variety of forms) about the importance of PPFP and the range of methods available. Document chosen method of contraception e.g. in the Maternity Case Record. DVDs or brief talks about PPFP can be provided in clinic waiting rooms. Posters emphasising the importance and advantages of PPFP should be available and visible. The woman’s choice should be communicated to the local community-based distribution (CBD) network, if available, so that a CBD worker can provide follow-up care as needed. Reminders should be placed in the antenatal record for providers to structure their discussion of PPFP options with women. |
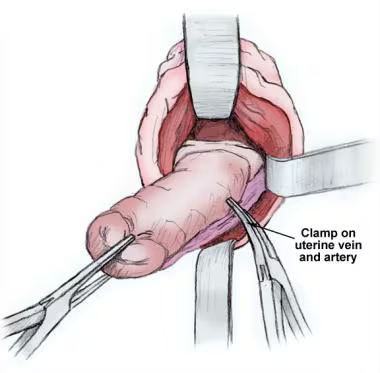
| In the labour ward | Women should be asked whether they have received contraceptive advice antenatally and, if so, the method they have chosen should be confirmed and then provided unless complications during pregnancy or delivery indicate the need for review. If the chosen method is not available in the labour ward, the method should be provided before the woman leaves the hospital or she should be referred to the most convenient place where the contraceptive method can be provided. Contraception should not be discussed with a woman who is in active labour. In women having a caesarean section, IUDs can be fitted as soon as the placenta has been delivered. Insertion is simple and expulsion rates are low. | Ensure that healthcare professionals (HCPs) who provide intrapartum care are trained to give contraceptive advice and to provide all methods, including IUD and implant insertion. Ensure that contraceptive implants and IUDs and the necessary equipment for their insertion are available at all times. |
| In the postnatal ward | If a woman has not had the chance to discuss contraception before she arrives on the postnatal ward, it should be discussed with her before she leaves the hospital Her chosen method (including an implant, or an IUD if within 48 hours of delivery) should be provided. | When women come in to the delivery suite too late in labour to discuss contraception. HCPs should raise the issue on the postnatal ward. HCPs on the postnatal ward should be competent to discuss all methods of contraception and to insert implants and IUDs. Ensure that all methods of contraception are available in the postnatal ward, including contraceptive implants and IUDs, and that the necessary equipment for insertion (including long forceps and a supply of IUDs) is available at all times. |
| In the postpartum care clinic/ In the baby immunisation clinic | Women attending for postpartum care should be asked whether they are using, or have a supply of, contraception. It should be confirmed with women who have chosen their method that they are happy with their choice, are knowledgeable about the method, have sufficient supplies and know where they can get more (if appropriate). If a woman has not chosen a contraceptive method, she should be told about all methods, particularly the most effective methods, and arrangements made to provide her with the method she has chosen. | Ensure that HCPs at baby immunisation clinics are trained to give contraceptive advice and to provide all methods, including implants and IUDs, or are able to refer appropriately. |
| In all settings | Ensure the involvement of all appropriate partners including CBD(community based) workers, midwives and peer educators. Facilitate training of all relevant staff in PPFP and particularly in IUD and implant insertion and follow-up care. Make every effort to avoid stock-outs of both contraceptives and the instruments required for IUD and implant insertion. Ensure that emergency contraception is available in all settings. Ensure that there are arrangements in place to facilitate timely access to vasectomy and interval female sterilization. |