A 29 year old married woman is referred to the gynaecology clinic for management of dysmenorrhea and dyspareunia. She has failed to conceive despite unprotected sexual intercourse for the past 1 year. Her menstrual cycles are regular.
She is otherwise healthy with a normal BMI. Findings of clinical examination are suggestive of endometriosis
1. Discuss the strengths and limitations of the investigations which could be performed on this patient. (35 marks)
2. Briefly discuss the treatment options you would propose for this patient. (65 marks)
Investigtions
Ultra sound scan
- – 1st line , freely available , no radiation risk , good sensitivity
- Detects ovarian endometriomas as unilocular, homogenous, thick walled cysts with low echogenicity (ground glass appearance)
- Bilateral ovaries may adhere together in midline (kissing ovaries)
- Hydrosalphinx may be seen as low-level echoes in dilated fallopian tubes
- Uterosacral ligaments barely detectable at USS may appear as Stellate hypoechoeic nodules located near the cervix.
- bowel endometriosis can be detected
- TAS- bladder emndometriosis
- can exclude other pathology – adenomyosis, fibroids
limitation >>>>
- Unable to detect superficial peritoneal endometriosis
- operator dependent , inter observer variation
- Helpful in deferentiating endometriomas from dermoid cysts
- transrectal scan is no superior to TVS
MRI
- Determines depth of bowel wall infiltration, length of affected area and distance of the lesion from anus
- Excellent in diagnosing bladder endometriosis (accuracy 98%).
- ureter involvement
limitation >>>
not freely available
not added advantages over TVS to detecting to detecting endometrioma
CA125
- non specific
- may supportive to diagnosis in the presence of clinical picture
- HSG –
- false positive rate is high
- not a option if suspecting underline pelvic pathology
but
- less invasive and less morbidity
- laparoscopy +/- biopsy
- gold standard
- positive histology confirm the diagnosis
- negative histology does not exclude it.
- theraputic at the same time
- can assess the tubal patency same time
- exclude other patholody – PID, adhesion, cyst
limitation
- invasive
- associated complication – surgical and anesthetic
- cost
- ovarian reserve – AMH and AFC – helpful for counselling and decide surgical procedures
Treatment option
two concerns – pain syndrome and infertility
- no place of medical managment – ovulation suppression is not acceptable here
- surgery is the corner stone of management of infertility due to endometriosis
- should manage in especialized center.
- MDT involvement – gynae surgeon, radiologist, necessary subspecialist – urologist , sergon
- pre op asessment – stenting , bowel preparartion
- consent
- intraoperative
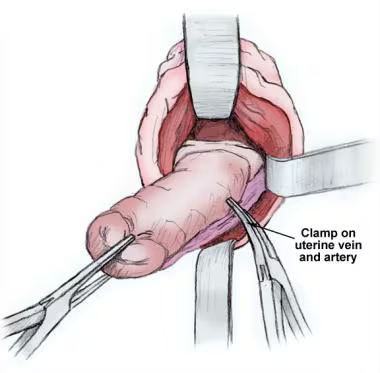
- adhesiolysis and restore pelvic anatomy
- excision of endometrial deposits – DIE – superior to ablation
- peritoneal – ablation – co2 better
- excision of endometrioms – superior to aspiration but may affect ovarian reserve
- bowel resection / ureter resection –
- minimal to mild – improve sponteneous pregnancy rate and live birth rate by surgery
- severe endometriosis – radical surgery – improve sponteneous pregnancy rate
- pre / post op ovarian suppression – not affect post op pain
- mild to modarate – IUI +COH in post op – improve live birth rate
- in severe endometriosis – poor prognosis of fertility
- need ART in form of IVF
- radical surgery will not improve IVF out come
- excision of endometrioma will facilitate oocyte retrival and reduce complications
- hyrosalphingx – saphyngectomy/ – improve IVF success
- GnRH – 3-6 cycle – will improve IVF out comes
- B/L tubal blockage / failed IUI following 6 cycle – IVF
- pain syndrome –