Discuss how you could improve the concept of safe motherhood in your area using the principles of risk management
Risk management refers to ‘the culture, processes and structures that are directed towards realizing potential opportunities whilst managing adverse effects’.
The basics of safe motherhood require:

The above pillars form the basis of improving the concept of safe motherhood which require prevention of:
- Maternal deaths
- Maternal morbidity due to near misses such as postpartum haemorrhage, severe sepsis and eclampsia
- Intrapartum and neonatal deaths
- Serious neonatal morbidity such as cerebral haemorrhage, fits and subsequent cerebral palsy
When applying the principles of risk management to reduce/prevent the above the following should be done
- risk identification.
We could either anticipate possible causes of risk before the event has actually happened (good antenatal care to detect serious complications early, monitoring during labour to prevent asphyxia at birth and early detection of PPH etc) or we could look back at things that did go wrong.
- risk analysis and evaluation
- risk treatment
- risk control/ monitoring
Also we should aim to
- Learn lessons from adverse incidents
- prevent recurrence
IN ACCORDANCE TO THE PRINCIPPLESS OF RISK MANAGEMENT AND SAFE MOTHERHOOD
- The main reasons for the above adverse incidents are:
- Failure to provide contraception till the woman is medically and emotionally fit to conceive.
- Failure to detect complications at the primary health care level
- Failure to provide good antenatal care.
- the delay in attending (delay 3) mainly due to inadequate staffing.
- Failure to scrupulously monitor the mother and the fetus during labour
- failure to provide guidelines (for management of normal and abnormal labour and obstetric emergencies etc) and failure to follow guidelines
- lack of required skills and knowledge at all levels of staff
- failure to identify serious conditions such as PPH, DVT, exlampsia and sepsis early
- failure of communications
- delay in reaching by the middle level staff and the consultant
- contributory factors which cause recurrence of adverse effects are
- poor documentation
- misplacement of documents such as BHT due to lack of an electronic data base with a secret password
- failure to conduct proper confidential inquiries for deaths and near misses
- absence of regular audits
- absence of regular training for all grades of staff
- poor leadership at the organizational and national level
To improve the concept of safe motherhood we should have preventive strategies for the factors in A and B.
One way of identifying what potentially could go wrong is to use a tool called Failure Mode and Effects Analysis (FMEA).In FMEA, a process is examined to identify what could go wrong and analyse the possible consequences of such failures
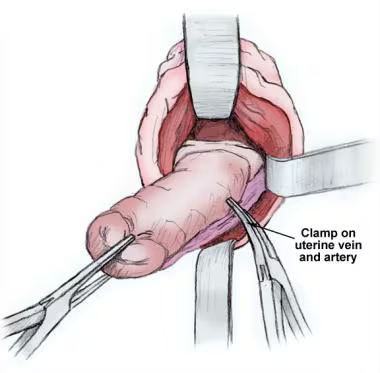
1 Examine a process in detail and outline every step. EX- management of labour, PPH, neonatal resuscitation
2. Identify ways in which any of the steps might go wrong; that is, the ‘failure modes’.
3. Establish the consequences (effects) of each failure mode.
4. Identify what could be the underlying causes (contributory factors).
5. Rate each contributory factor and/or failure mode in terms of its frequency or likelihood of occurrence and each effect in terms of the severity of its consequences.
6 Identify any existing ‘controls’ (factors acting to prevent, detect, monitor or mitigate this risk).
7. Use the ratings to prioritise risks; decide which risks to accept and which ones to treat.
8. Devise an action plan
Risk is best managed not in isolation but within a framework that integrates all aspects.
The unit should practise a safety culture and provide the necessary resources. A safety culture is more likely to flourish where there is strong leadership, teamwork, communication, user involvement and training.
Staffing and staff management are an integral part of clinical governance, risk management and safe motherhood
Well cared and motivated staff who are not tired due to long working hours are likely to perform better and less likely to make mistakes. Staff should have a safe working environment and culture that provides adequate rest, comfort, and meal breaks.
Increased involvement of consultant obstetricians in the labour ward and in the care of women with complicated pregnancies and in the supervision and education of medical staff is important .
Resources, facilities and staffing should be matched with the workload.
All maternity admissions should be seen immediately.
There should be scrupulous monitoring during labour with adherence to protocols.
Proper handing over and taking over by all grades of staff is essential to improve patient care and to reduce risks.
There should be a written risk management strategy and a designated risk lead. Leadership should be provided by a multidisciplinary risk management or clinical governance committee. Membership should include a senior obstetrician (risk lead) as well as a training-grade doctor, a midwifery nurse, an anaesthetist and a neonatologist.
Team work within the unit with the participation a of all grades from the cleaner to the consultant is essential . Multi-disciplinary team work should be available depending on the care required for each individual case.
Leadership is an essential part of risk management and safe motherhood. In Sri Lanka leadership is provided by the Minister, Director General, provincial director, hospital director and the relevant consultants.
Communication failures especially within various grades of staff within the unit result in risk incidents and adversely affect patient care.
There should be reliable telephone services and frequent methods of communication :
- Within the staff of the unit.
- With patients to get a feed back and learn from our mistakes.
- With primary care units(MOH)
- With external agencies (mental health services, child protection society, women wellbeing society ).
- With strategic planning units (ministry of health, SLCOG)
There must be effective collaboration with the local and national, maternal, neonatal and child health services.
Peripheral health services should function well with every woman attending the pre—conception and antenatal clinics and early referral of high risk patients to tertiary care centers.
Family planning clinics should be available at all health care facilities and suitable contraception should be provided till the woman is mentally, socially and medically fit for pregnancy.
Gender based violence, gender inequality and substance abuse should be detected by the midwife and remedied by combined efforts of the medical staff and the government.
Staff should be continuously updated and equipped with the latest knowledge and skills required to .
- Do research and audits
- manage obstetric emergencies
Models should be available for training (ventouse and forceps deliveries, shoulder dystocia)
CME would be an integral part of the appraisal and job recruitment process
From previous experiences of adverse events:
- Create a database to identify common patterns of adverse events
- Develop systems of accountability to prevent future events
Confidential inquiries into Maternal and perinatal deaths should be properly conducted as soon as possible after the event with the availability of all documents and participation of key personnel. Inquiries should also be conducted for near misses such as eclampsia, serious PPH requiring massive transfusion and hysterectomy, pulmonary embolism, shoulder dystocia, third and fourth degree perineal tears, failed instrumental deliveries, birth trauma, neonatal fits, etc. Remedial action should be recommended and followed. There should be audits and inspection visits twice a year to supervise each unit so that risks and mistakes can be corrected early.
Finally ‘umbrella’ term encompassing several themes and processes that together ensure an environment in which clinical excellence will flourish should be considered to improve the concept of safe motherhood. A patient can be imagined standing under the umbrella that is created by the interaction of all persons and processes which ensure the safety and quality of patient care and any failure or deficiency is likely to cause ‘leaks’ in the umbrella that may adversely affect patient’s right to safe motherhood.