Discuss the causes and management of a 6 months old infant with ambiguous external genitalia
Ambiguous eternal genitalia occur as a result of under masculinisation of an XY individual or virilisation of a XX individual. This can be caused by:
- Gene mutations/chromosomal abnormalities
- Inappropriate hormone levels
- End organ resistance
If palpable gonads are present the infant is an undervirilised male.
Ambiguous external genitalia can occur as a result of
- Sex chromosome DSD—
Chimera karyotypes (46XX/46 XY)
- 46 XY DSD –
Undervirilisation of 46 XY individuals
Causes
- A defect in expression of 17β-Hydroxy dehydrogenase steroid 3
Results in the inability to convert androstenedione to testosterone. The external genitalia are atypical or of female phenotype because of insufficient testosterone and, consequently, DHT. AMH cause regression of mullarian structures and male internal genitalia occur due to presence of isoenzymes of 17β-HSD3
- 5 alpha reductase deficiency, preventing the conversion of testosterone to DHT.
In 5AR deficiency, the karyotype is XY, the gonads are testes, müllerian structures have appropriately regressed with the presence of AMH and the wolffian ducts have developed into male internal reproductive tracts under the influence of testosterone. The external genitalia, however, have developed in the female-specific pattern in the absence of DHT.
- 46XY ovotesticular DSD
- Resistance of the androgen receptor or its mediators to the binding of testosterone and DHT results in partial insensitivity.
- Complete androgen insensitivity may be diagnosed as ambiguous external genitalia if the testes are palpable in the “vulva”.
- 46 XX DSD
Masculinisation of XX females
Causes
- 46XX ovotesticular DSD- true hermophrodites
- Virilisation caused by androgen excess ( commonest is CAH);
- Exposure to exogenous androgens in utero
Maternal androgen secreting ovarian tumours
Maternal adrenal tumours
Maternal drugs
Fetal tumours which produce androgens
- Placental aromatase deficiency
Diagnosis
Diagnosis includes taking a history, examination, biochemical analysis, genetic scrutiny,
imaging and possible surgical exploration and biopsy
History
Obstetric history
- Drug exposure
- History of androgen secreting tumours or adrenal disorders
- Prematurity as the clitoris will be more prominent and testes will be undescended
- History of previous unexplained neonatal death, stillbirth, multiple miscarriage
- infertility
Family history
- Congemital abnormalities and dysmorhic features
Examination
Examination of the external genitalia includes assessment for the location of palpable gonads, position and presence of urethral meatus, degree of fusion of the labio-scrotal folds, presence of a vaginal opening separate from the labioscrotal folds and size of the clitoris
Investigations
Karyotyping is the first investigation.
46XX
Further tests and diagnosis of the cause
- First step is to exclude CAH by performing 17 hydroxy progesterone levels and urinary steroid profile If positive exclude a life-threatening salt-wasting crisis. Perform tets to establish the following:
- Serum electrolytes
- Plasma glucose
- If negative consider maternal source of androgens ( ovarian tumour , adrenal tumour, use of drugs with an androgenic effect) or placental aromatase deficiency. Perform adenal hormones and testosterone levels in the mother. Perform USS to exclude ovariam and adrenal tumours.
- Perform USS of the neonate for internal genitalia and gonads and to exclude a hormone secreting tumour. MRI may be needed
- Laparoscopy and gonadal biopsy should be done to exclude true hermaphroditism.( XX/XY mosaic)
46XY
Investigations
- hCG stimulation test followed by testing levels of testosterone, androstenedione and DHT, – poor testosterone response may due to lack of 17hydroxysteroid dehydrogenase or a block in conversion to DHT due to 5 alpha reductase deficiency.
- Testosterone levels
- Gonadotropin levels
- AMH levels to determine the presence of testicular tissue. AMH levels are a marker of Sertoli cell function and, as such, can differentiate between those without functioning testicular tissue and those with androgen biosynthetic defect or insensitivity
- USS for internal genitalia and inguinal gonads
- Laparoscopy and gonadal biopsy
Ovotesticular DSD – true hermophraditism
- May have a mosaic karyotype XX/XY
- Perform laparoscopy and gonadal biopsy
Management
Carried out in a Tertiary centre
(MDT) approach is necessary. Should include a consultant paediatrician with subspecialists in endocrinology, surgery, urology, genetics, neonatology, psychology/ psychiatry, gynaecology and medical ethics.
Psychosocial management is required to promote positive adaptation.
- Gender assignment
Avoid gender assignment before expert evaluation of the newborn.
However, it should be made as soon as diagnostic evaluation permits.
Factors which influence gender assignment are:
- Diagnosis of the abnormality
- Genital appearance
- Therapeutic options and prospects of surgical correction
- Need for life long replacement therapy,
- Potential for fertility and sexual function,
- Views of the,family,
- Sometimes circumstances relating to cultural practices.
Recommendations are to raise infants with:
- 46,XY complete androgen insensitivity syndrome, 46 XY gonadal agenesis and 46,XX CAH as females.
- 46 XY 5a-reductase as males – At puberty, alternative isoenzymes that are capable of converting testosterone to DHT are produced, resulting in virilisation of the external genitalia.12 Antenatal and postnatal exposure of the brain to testosterone is thought to contribute to a male gender identity in many individuals with 5AR deficiency
- 17-hydroxysteroid dehydrogenase-3 deficiency as males. At puberty, increasing levels of LH result in higher levels of androstenedione, which is converted by isoenzymes in extragonadal tissues to testosterone. This causes the development of male secondary sexual characteristics, such as growth of the external genitalia, increased muscle mass, body hair and deepening of the voice.
- 46 XY gonadal dysgenesis, partial androgen insensitivity and true hermaphrodites may be reared as males or females depending on the degree of virilism.
2.Hormone replacement
- Those reared as males will need testosterone for pubertal development and to maintain bone mineral density.
- Complete recovery occurs with treatment in congenital adrenal hyperplasia and hormone replacement is not necessary.
- Those with 46,XY complete androgen insensitivity syndrome and 46 XY gonadal agenesis will be reared as females and may need oestrogens for 1—2 years at the time of puberty for breast development ( may not be necessary for CAIS if good breast development is present) followed by HRT for life. ( combined HRT for gonadal agenesis as the uterus is present and oestrogen only for complete androgen insensitivity as the uterus is absent)
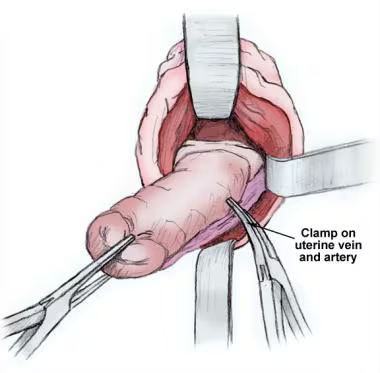
3 surgical treatment
- May be done during infancy to allow adaptation and to avoid stigma.
- However further corrections may be needed after puberty.
Surgery in those reared as males:
Correction of hypospadias
Surgery in those reared as females:
- Clitoral reduction
- Separation of fused labia
- Urogenital sinus repair
- Vaginal reconstruction and dilatationis done later
4.Excision of the gonads
Risk of gonadal malignancy is high in those with a Y chromosome. Risk is highest in those with gonadal dysgenesis and PAIS with abdominal gonads. Risk is lower with CAIS and the gonads are removed after breast development is complete because testicular oestrogens play a role in breast development