Borderline ovarian tumor.
Q. A woman comes with a history report of a borderline ovarian cyst. How will you manage.
Theory TOG
- What is a boarderline ovarian tumor?
Distinct pathological group of neoplasms that demonstrate higher proliferative activity but
which do not show stromal invasion. Also known as tumors of low malignant potential.
Constitute 10-15% of all epithelial ovarian neoplasms.
Typically seen in younger women. - What is the 5 year survival rate?
a. For stage I – 95%-97%.
b. Stage III – 50-86%. - What are the risk factors?
a. Younger women
b. Nulliparous
c. Lactation protective
d. OCP is not protective
e. No evidence of BRCA mutations increasing the risk.
f. Mutation of BRAF/KRAS pathway (high grade P53) - What are the histological features
a. Serous borderline are the most common type. (50%)
b. B/L in 30%.
c. Can be associated with extra ovarian lesions (implants) = can be invasive or
non inasive.
d. Mucinous borderline aconstitute 46%. Further classified into
i. Intestinal 85%
ii. Endocervical/ Mullerian 15%.
- Associated with peritoneal pseudomyxoma in 10% and can be
indistinguishable from primary appendiceal tumors, necessacitating a
thorough investigation of the GI tract with special attention to the
appendix.
e. Mixed, endometrioid, clear cell and brenner – 4%
Histological features are defined by epithelial cellular profileration hreater than that seen in
benign tumors. They have a stratified epithelium with varying degrees of nuclear atypia and
increased mitotic activity and lack of stromal invasion.
Diagnosis
Borderline ovarian tumours are more likely to be asymptomatic and to be diagnosed as an
incidental finding or at routine examination.
Longer duration of symptoms.
Pelvic pain, bloating, dyspareunia, menstrual irregularities, pressure symptoms.
CA125 maybe raised. 19.9 maybe elevated in mucinous.
RMI often low.
TVS – cyst characteristics. Complexity.
Doppler – intracystic blood flow
A wide variety of appearances, ranging from unilocular cysts, minimally septate cysts with
papillary projections and markedly septate lesions with plaque-like excrescences to solid
lesions with exophytic papillary projections, can be demonstrated on magnetic resonance
imaging (MRI).
Management
- Management depends on age, stage, potential desire for pregnancy and nature of
peritoneal implants. - Standard management is similar to that of invasive ovarian cancer: namely, accurate
staging and cytoreductive surgery where appropriate. - Where possible, ovarian tumours should be subjected to frozen section analysis.
- If the frozen section is reported as borderline, for the older woman with no fertility
concerns a complete staging should be undertaken, which should include:
a. exploration of the entire abdominal cavity with peritoneal
washings
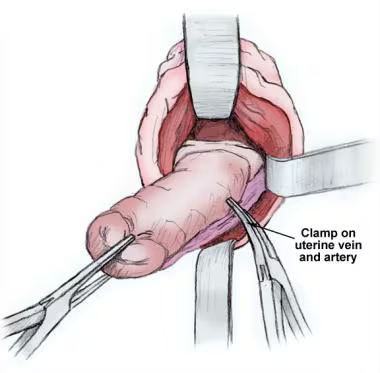
b. total abdominal hysterectomy
c. bilateral salpingo-oophorectomy and infracolic mentectomy
d. appendicectomy in the case of mucinous tumours.
Approximately one-third of cases reported as borderline at frozen section are later
reclassified as invasive tumours.
no survival benefit has been shown with lymphadenectomy.
When a borderline tumour is diagnosed on histology after primary surgery, a referral to the
regional cancer centre followed by discussion at the local multidisciplinary team meeting
may be useful.
The role of restaging and completion surgery
The decision to undertake further surgery will largely be determined by three factors: the
histological subtype of borderline ovarian tumour, the completeness of the primary surgery
and the fertility desires of the woman.
Risk increases when there are invasive implants (31% vs 21%)
Presence of DNA aneuploidy 19 fold risk.
Restaging may be warranted for women with micropapillary tumours, invasive implants or
DNA aneuploidy and those with no fertility concerns.
There is less justification for further surgery for a woman who has undergone full
laparotomy with inspection of all surfaces at primary surgery.
The role of conservative surgery and subsequent fertility - For early stage – conservative surgery is an option. – defined as Surgery with
complete staging but with preservation of the uterus and at least a part of one ovary
to preserve fertility. Two common options
a. Cystectomy
b. Unilateral SO +/- infracolic omentectomy and peritoneal washings.
c. - Counsell regarding risk of recurrence and subsequent fertility.Relapse rate
a. Cystectomy – 12-58%
b. SO- 0-20%
c. Radical surgery – 2.5-5.7%.
d. Counsell about the importance of long term follow up.
e. No adverse effects on pregnancy on the disease or vice verca.
f. Spontaneous fertility rate of 32-65%. - Need for removal of remaining ovary and uterus once the family is complete is
debatable.
a. Because recurrence is easily resectable, one can wait for the recurrence.
b. But because of psychological stress women will chose to have definitive
treatment upon family completion. - Role of laparoscopy -should ideally staged by a midline laparotomy.
- Role of chemotherapy – No role for adjuvant chemotherapy.
- Follow up .
a. Done conservative surgery – clinical examination, TVS – every 3 months for 2
years, every 6 months for next 2 years and annually thereafter