A 46-year-old woman attends the Well Women Clinic asking for advice on contraception.
(a) Evaluate her contraceptive options.
(b) How will her age
influence your recommended method?
(c) What factors in her history will be against her use of LARCs?
Common mistakes
● Details of hormone replacement therapy (HRT) in a perimenopausal woman
● Advantages of HRT
● Diagnosis of menopause
● Contraindications to HRT
● Screening for cervical/endometrial cancer
● Contraception in a perimenopausal woman in general
● Measuring cholesterol levels and discussing their importance
A good candidate will include some or all of these points
(a) Evaluate her contraceptive options.
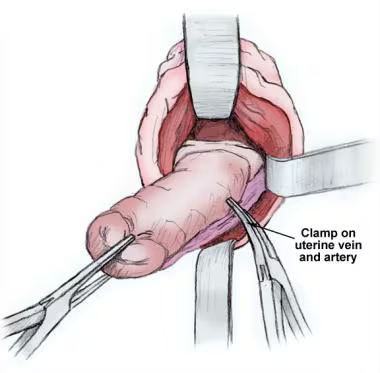
● —-Sterilisation—-consider permanent, one-off procedure, complications of surgery and
anaesthesia risk of ectopic if failure,
failure rate
Female sterilisation. 1:200
vasectomy 1:2000
●— LARCs—– – Mirena, IUDs, Depo-Provera, Implanon – reduced dependence on patient
compliance:
● More effective at the end of reproductive life
● Need to exclude contraindications
● ——–COCP—-
● If non-smoker and not obese
● No contraindications
● Could provide additional benefits as HRT
● Increase risk of venous thromboembolism (VTE)
(b) How will her age influence your recommended method?
● Older therefore fertility lower and efficacy of all methods better
● More likely to have medical problem which will be a relative contraindication to some
of the methods
● More likely to be in a stable relationship, hence reduced risk of PID
● More like to accept sterilisation
● Periods more likely to be irregular, hence contraceptive that may help this likely to be
acceptable
● Perimenopausal, hence contraception may act as HRT
(c) What advice will you give about contraception and HRT?
● Contraception important as pregnancy can occur – hormone levels do not exclude the
risk of pregnancy
● Age <50 – contraception for 2 years after age 50
● Age >50 contraception for 1 year
● On HRT before menopause – stop and wait for 6 months, then check hormone
levels/remains amenorrhoeic
● IUD, surgical sterilisation, COCP
Sample answer
(a) Evaluate her contraceptive options.
The options include tubal ligation (sterilisation), the COCP, the mini-pill and LARCs such as
the IUD, Depo-Provera, Mirena and Implanon.
Tubal ligation (sterilisation) is an ideal method for any age group.
In the perimenopausal woman, this is even more ideal and it is unlikely that she will return requesting for reversal.
However, during counselling, the frequent occurrence of irregular periods in this age group
must be emphasized, as some women may blame the irregularity of their periods on the sterilisation.
The failure rate of female tubal ligation is 1:200 compared to 1:2000 for vasectomy.
The latter is easier to perform and has fewer side-effects and complications. It can also be performed under local anaesthesia.
The COCP is another option. The low-dose oestrogen COCP will be more suitable in this
age group. However, since this is associated with an increased risk of VTE, the risk factors for
this complication, such as smoking, obesity, hypertension, family history and thrombophilia,
must be excluded. Again, this is more effective in this age group. It may provide the added
benefit of counteracting perimenopausal symptoms, which may require HRT. The mini-pill is an effective form of contraception however, the complication of irregular vaginal bleeding may cause unnecessary anxiety derived from the need to exclude hyperplasia or endometrial carcinoma.
However, the mini-pill may offer relative protection against oestrogen-induced
endometrial hyperplasia. For this option, compliance is an important factor.
The LARCs, just like all forms of contraception, are more effective in this age group compared to younger women. However, they must be acceptable to the patient. The first in this
group are the IUDs (copper medicated or the Mirena). The complication of irregular vaginal bleeding, especially during the early months after administration, may result in early discontinuation, especially with Mirena.
For most women, adequate counselling will result in a high
continuation rate. Since the duration of this form of contraception depends on the type of LARC, the choice could be such that, once administered it potentially covers the rest of the reproductive life of the woman. The irregular vaginal bleeding with this method may require investigating and therefore generate significant anxiety. For women who also need HRT, the Mirena may be combined with HRT to offer endometrial protection.
(b) How will her age influence your recommended method?
The efficacy of any chosen method of contraception is higher in the older woman as fertility
declines.
The permanent form of contraception is more acceptable to older women, who are
more likely to have medical problems such a diabetes mellitus and hypertension which may be
considered relative contraindications to some forms of contraception.
The older woman is at
risk of VTE and added risk factors such as smoking will limit the choice of method.
Advancing age is associated with irregular periods which are themselves a relative contraindication to
some forms of contraception. However, having said that, the older woman is more likely to accept irregular vaginal bleeding and other side-effects of contraceptives. The chosen methods may also induce amenorrhoea more easily in these women. Finally, the timing of replacements of various options may differ significantly because of reduced fertility.
(c) What advice will you give about contraception and HRT?
Contraceptive advice is extremely important in the woman who is on cyclical HRT or is about
to start HRT and is perimenopausal. She should continue with an adequate form of contraception for up to 2 years after the presumed age of menopause.
As this is difficult to ascertain, it may be advisable for the woman to stop HRT and contraception for 6 months and see whether her periods resume, or measure hormone levels and ascertain that ovulation does not occur.
Stopping contraception in these women could be extremely difficult. In those who are
under 50 years of age, it is advisable to continue contraception for 2 years after the age of 50
before stopping, and for those over the age of 50, continuation should be for 1 year.